Imagine living in a world where your thoughts race endlessly, and focusing feels like an impossible dream. This is the daily reality for many people with ADHD. Amidst the struggle to keep up with life’s demands, a shadow often looms depression. How are these two conditions connected? And what does this mean for those who navigate the challenges of ADHD?
In today’s post, we will explore the intricate link between ADHD and depression. We will explain why they often coexist and what you can do about it. Join us on this journey to better understanding and hope. By the end, you’ll grasp the depth of this connection and discover strategies for a brighter, more empowered future.

Understanding ADHD: More Than Just Inattention
ADHD is more than just an inability to focus. It involves a range of symptoms that affect daily life. People with ADHD often struggle with impulsivity, restlessness, and difficulty organizing tasks. These challenges can make even simple activities feel overwhelming.
Recognizing these symptoms is the first step to understanding ADHD. It’s important to know that ADHD affects both children and adults. While children might be hyperactive, adults might feel more internal restlessness and anxiety. Awareness can lead to better support and management.
Effective management of ADHD requires a comprehensive approach. This includes medication, therapy, and lifestyle changes. Cognitive-behavioral therapy (CBT) can help in developing coping strategies. Medications, such as stimulants, can improve focus and control impulsivity.
Creating a supportive environment is crucial for those with ADHD. Simple changes, like breaking tasks into smaller steps, can reduce overwhelm. Encouraging regular exercise and a healthy diet can also improve overall well-being. With the right strategies, people with ADHD can lead fulfilling, productive lives.
The Hidden Link: How ADHD Can Lead to Depression
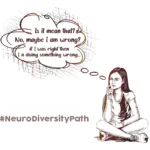
ADHD and depression often occur together, creating a complex emotional landscape. The constant struggle to manage ADHD symptoms can lead to feelings of frustration and failure. Over time, this can erode self-esteem and lead to persistent sadness or hopelessness. The relentless demands of keeping up can make the future seem bleak.
Understanding this connection is key to addressing both conditions effectively. People with ADHD are more likely to experience negative feedback from peers, teachers, or colleagues. This can increase stress and anxiety, paving the way for depression. Recognizing the signs early can help in seeking appropriate treatment before the depression deepens.
Combining treatments can offer significant relief. Cognitive-behavioral therapy (CBT) is effective for both ADHD and depression, helping individuals develop coping mechanisms and reframe negative thoughts. Medication may also be necessary to manage severe symptoms. By addressing both conditions simultaneously, individuals can improve their mental health and quality of life.
Recognizing the Signs: Symptoms of Depression in Those with ADHD
Recognizing the signs of depression in individuals with ADHD can be challenging. Depression symptoms often overlap with ADHD, making it hard to distinguish between the two. Common signs include persistent sadness, loss of interest in activities, and fatigue. In those with ADHD, these symptoms might be mistaken for typical ADHD behavior, like inattention or lack of motivation.
Awareness of specific indicators can help in early identification and treatment. For instance, increased irritability, social withdrawal, and changes in sleep patterns can signal depression. Pay attention to complaints of feeling worthless or excessive guilt, as these are critical red flags. Recognizing these signs early can prompt timely intervention, which is crucial for effective treatment.
Seeking professional help is essential for accurate diagnosis and treatment. Mental health professionals can distinguish between ADHD and depression symptoms, ensuring appropriate care. A combination of therapy and medication often works best. Family support and education about both conditions can enhance understanding and provide a strong foundation for recovery. Identifying and addressing depression promptly can significantly improve the overall well-being of those with ADHD.
The Emotional Toll: Why ADHD Can Trigger Feelings of Despair
The emotional toll of ADHD can trigger profound feelings of despair. Constantly struggling to meet expectations and facing frequent criticism can weaken one’s resilience. This ongoing battle often leads to chronic stress and anxiety, creating a fertile ground for depression. The persistent feeling of not measuring up can be devastating.
Research highlights the significant impact of ADHD on emotional health. A study conducted by Dr. Margaret Weiss at the University of British Columbia found that individuals with ADHD are at a higher risk for depression and anxiety disorders. The study underscores the importance of recognizing the emotional challenges faced by those with ADHD, as untreated emotional distress can exacerbate both conditions.
Addressing these feelings involves understanding their roots and seeking targeted support. Cognitive-behavioral therapy (CBT) can help individuals reframe negative thoughts and build coping strategies. Support groups also provide a sense of community and shared experiences, reducing feelings of isolation and despair.
Building resilience is key to managing ADHD and its emotional toll. Encouraging self-compassion and celebrating small achievements can boost self-esteem. Mindfulness practices, such as meditation and deep-breathing exercises, can also alleviate stress. By fostering a supportive environment and seeking appropriate treatment, individuals with ADHD can navigate their emotional challenges more effectively and lead fulfilling lives.
Strategies for Hope: Managing ADHD and Depression Together
Comprehensive Treatment Plans
Managing ADHD and depression together requires a comprehensive treatment plan. This plan often includes a combination of medication, therapy, and lifestyle changes. Stimulant medications can help manage ADHD symptoms, while antidepressants may be prescribed for depression. Working with healthcare providers to find the right medication balance is essential. Regular follow-ups and adjustments ensure the treatment remains effective and minimizes side effects.
Cognitive-behavioral therapy (CBT)
Cognitive-behavioral therapy (CBT) is a highly effective approach for both conditions. CBT helps individuals identify and challenge negative thought patterns, replacing them with more positive and realistic ones. This therapy can improve emotional regulation and problem-solving skills. For those with ADHD, CBT can also address organizational and time-management difficulties, enhancing overall functioning and reducing feelings of overwhelm.
Lifestyle and Support
Incorporating healthy lifestyle habits and building a support network are crucial strategies. Regular physical activity, a balanced diet, and sufficient sleep can significantly impact mood and cognitive function. Mindfulness and relaxation techniques, such as yoga or meditation, can help manage stress and anxiety. Joining support groups or connecting with others facing similar challenges provides emotional support and practical advice. By integrating these strategies, individuals can manage both ADHD and depression more effectively, fostering a sense of hope and resilience.
Seeking Support: Resources and Help for Navigating Life with ADHD and Depression
Seeking support is vital for managing ADHD and depression effectively. Professional guidance from psychologists or psychiatrists is essential for tailored treatment plans. A study by Dr. Russell Barkley at the Medical University of South Carolina emphasizes the importance of comprehensive care, which includes therapy, medication, and lifestyle adjustments. Accessing mental health professionals who specialize in ADHD and depression ensures that individuals receive nuanced and effective care. Online resources, such as the websites of CHADD (Children and Adults with Attention-Deficit/Hyperactivity Disorder) and the Anxiety and Depression Association of America (ADAA), offer valuable information and support networks.
Building a strong personal support system can make a significant difference. Family and friends who understand the challenges of ADHD and depression can provide emotional support and encouragement. Educational workshops and support groups, both in-person and online, can connect individuals with others facing similar struggles, fostering a sense of community. Utilizing resources like ADHD coaches can also help develop personalized strategies for daily challenges. By leveraging these supports, individuals can navigate the complexities of ADHD and depression with greater confidence and resilience.
“Asking for help is the first step. You are more precious to this world than you’ll ever know.”
– Lili Rhinehart
In exploring the connection between ADHD and depression, we’ve highlighted the complexities and emotional challenges that many face. Understanding ADHD beyond its surface symptoms reveals why depression often accompanies it. Recognizing the signs and addressing the emotional toll can lead to effective management strategies. Combining comprehensive treatment plans, cognitive-behavioral therapy, and supportive lifestyle changes fosters hope and resilience. Seeking professional support and building a strong personal network is crucial for navigating life with both conditions.
Reflecting on this article, I’m reminded of the importance of empathy and awareness. The struggles of ADHD and depression are profound, but with the right tools and support, a brighter future is possible. Let’s continue to learn and support each other in this journey.
Your experiences and insights are valuable. Please share your thoughts or ask questions in the comments below. Together, we can create a supportive community.